Zimmer Total Ankle Replacement Reviews Vs Hintermann Series H2ã‚â® Total Ankle Replacement System
- Research article
- Open Access
- Published:
Early clinical and radiological evaluation in patients with total ankle replacement performed by lateral approach and peroneal osteotomy
BMC Musculoskeletal Disorders volume 20, Article number:132 (2019) Cite this article
Abstract
Background
The Zimmer Trabecular Metal Total Ankle Replacement (Zimmer TM TAR) is a recent talocrural joint arthroplasty canonical for use in the U.s.a. and Europe. Many of the studies reporting the results of this implant are provided by surgeons involved at least in the initial blueprint of the implant under study.
The aim of this study is to depict the early on clinical and radiological outcomes in patients who underwent this process performed by not-designer surgeons.
Methods
A total of thirty consecutive patients underwent total ankle replacement with a Zimmer TM TAR surgery betwixt July 2013 to January 2016.All clinical assessments were collected pre- and mail service-operatively with minimum follow-up of 12 months for each patient using the American Orthopedic Human foot and Ankle (AOFAS) score, the Foot Role Index (FFI) and a visual analogue scale (VAS) for pain. Radiographic outcomes included ankle orientation assessed with bending "α","β" and "γ" according to Wood. Furthermore, the anteroposterior offset ratio was measured in weight-begetting lateral ankle radiographs at the terminal follow-upwardly.
Results
The mean preoperative FFI-pain (FFI-P) value was 53.67, the FFI-disability (FFI-D) was 64.19. At the last follow-up visit, the FFI-P and FFI-D was 16.95 and xx.76 respectively (p<0.01 for the both scales). Preoperatively, the mean VAS for pain and AOFAS score was vii.81 and 40.95 respectively, and at the last follow-upwards 2.29 and 86.38 (p<0.01 for the both scales). The mean bending calculated using Woods and Deakin's method were "α"= 89.02°, "β"= 85.eleven and "γ"= 27.54 post-operatively. At the concluding follow-up the aforementioned values were respectively 89.43, 85.18 and 29.94. At the last follow-up, the mean outset ratio was 0.06 (range 0.003/-0.17).
Conclusions
These early results show high levels of patient satisfaction, and nosotros are encouraged to continue with lateral approach total talocrural joint arthroplasty.
Background
Numerous studies reported the efficacy of new third-generation of total talocrural joint arthroplasties for the treatment of advanced ankle osteoarthritis with clinical results comparable to ankle arthrodesis [one, ii]. The improvement in noesis of talocrural joint joint biomechanics, instrumentation, surgical approach may led to even college clinical results in comparison to arthrodesis. The Zimmer Trabecular Metallic Total Ankle Replacement (Zimmer TM TAR) is a recent ankle arthroplasty canonical for utilise in the United states of america and Europe. The implant requires a lateral approach and a peroneal osteotomy. Potential advantages with a trans-fibular arroyo included the direct visualization of the center of rotation of the ankle and a theoretical reduced take a chance of wound complications due to exposure of the ankle joint through a surgical plane between angiosomes. Furthermore, this approach allows the surgeon to address coronal rotational and sagittal plane and provides a more physiological orientation of the tibia and talar component.
Many of the studies reporting the results of this implant are provided past surgeons involved at least in the initial design of the implant under written report [iii]. Thus, familiarity with the system tin can be a potential bias affecting outcomes and orthopedic surgeons may find difficulties in reproducing the results.
The aim of this report is to depict the early clinical and radiological outcomes in patients who underwent this process performed past not-designer surgeons.
Methods
This retrospective written report was approved by our upstanding commission (San Raffaele Hospital, 76/int/2017) and a written informed consent was obtained from all patients.
A group of thirty consecutive patients who underwent full ankle replacement with a Zimmer TM TAR surgery between July 2013 to January 2016 was unrolled in this study. Indications for TAR were end-staged osteoarthritis of the ankle (main, secondary, or post-traumatic) with good os stock, neutral alignment or mild-to-moderate malalignment, skillful stability, and preserved motion of the ankle. Preoperative hindfoot malalignment was not considered an accented contraindication, but additional surgical steps (supramalleolar and/or calcaneal osteotomies, ligament reconstruction, subtalar arthrodesis) was performed to correct the deformity.
There were 11 women and 19 men. The mean age was 58.ii years (range 22-77). The mean follow-up was 29.7 months (range 18-49).
Indications for surgery were mainly represented by post-traumatic osteoarthritis, secondary ankle osteoarthritis to giant prison cell tumor of the tendon sheath (GCT-TS), i rheumatoid arthritis and one primary osteoarthritis. Fifteen patients had mail service-traumatic osteoarthritis secondary to ankle fracture while xi patients had mail service-traumatic osteoarthritis secondary to ligament injuries. The patient with ankle osteoarthritis secondary to GCT-TS category refused an ankle fusion, and even though he had 22 years at surgery, we performed tumour removal and TAR. Routinely, nosotros are against TAR in young adult patients, but the strong will of the patient forced us to change indication. The patient was also fully informed about the theoretical survivorship of the implant and the possible future treatments in instance of failure or GCT-TS recurrence.
Patients with neuropathy, diabetes, excessive bone loss (>l%) due to avascular necrosis or trauma, recent history of septic arthritis or obese (BMI>30kg/one thousand [2]) were considered not suited for this blazon of surgery and therefore underwent different treatments.
Exclusion criteria included incomplete records, a lack of adequate follow-upwardly duration and the use of different implants.
All clinical assessments were collected pre- and post-operatively with minimum follow-upwards of 12 months from each patient using the American Orthopedic Foot and Ankle Society (AOFAS) score, the Foot Function Alphabetize (FFI) and the visual analogue scale (VAS) for pain [4, 5]. Patients were as well asked to appraise their satisfaction with the surgical upshot based on a three-grade scale: very satisfied, satisfied or not satisfied with the consequence. The range of movement (ROM) was evaluated using a goniometer by one of the investigators (JF).
Standard (anterior-posterior and lateral) weightbearing radiographs of the ankle were collected pre-operatively and at the final follow-up for all patients and independently evaluated past 2 orthopedic surgeons (AB, JF). These radiographs were assessed for the presence of aseptic loosening (i.e. radiolucency > 2 mm in width, bone cysts at the margin of a component or migration of a component [vi]). The components alignment was checked with the method past Woods and Deakin, either post-operatively and at the last follow-upwardly using three athwart measurements (α, β and γ) (Fig. ane) [7].
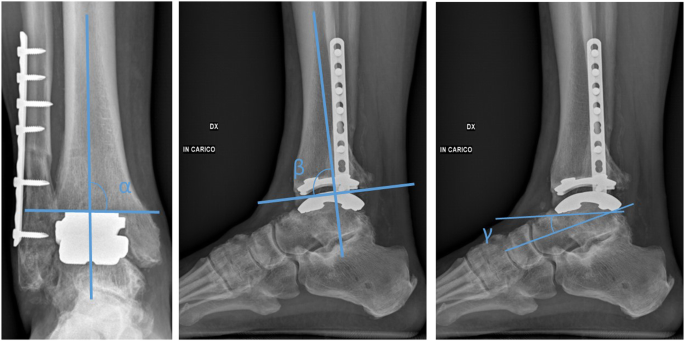
Radiographic angles (α, β, γ) for assessment of components position and migration
A change in positions bigger than 3° relative to the long axis of the talus, assessed on the lateral radiograph ("γ") was considered sign of loosening. Furthermore, the anteroposterior commencement ratio was measured in weight-bearing lateral talocrural joint radiographs at the last follow-upward [viii]. Positive values were defined when the center of the circle was anterior to the tibial centrality and negative values when posterior to the tibial axis.
Surgical technique
The surgical technique was carried out following to the manufacturer's guidelines with the original Zimmer TM TAR instrumentation. An oblique osteotomy (superolateral to inferomedial) starting approximately ii.5 cm proximally to the ankle joint line is performed. The anterior talofibular ligament (ATFL) is sectioned sparing enough tissue to perform reconstruction at the end of the implantation. The posterior capsule and ligaments are then released. Osteophytes in the medial gutter and any anterior osteophytes can be managed through a small incision medial to the anterior tibial tendon. The leg is then placed in the alignment frame and the alignment is checked on anteroposterior and lateral fluoroscopy. The os resection is completed using the cutting guide and a rotational burr. The prosthesis is implanted co-ordinate to previous intraoperative measurements with regard to prosthesis size in both frontal and sagittal planes. Fibular osteotomy is and so stock-still with plate and screws. Later on fibular fixation, the ATFL was repaired. After surgery a short leg cast is fabricated, and weight-begetting is prohibited for 1 month. At the terminate of this flow the bandage is removed and partial weight-begetting is allowed for 2 weeks. At 6 weeks from surgery weight-bearing is immune without restrictions and rehabilitation with a physiotherapist is encouraged.
Statistical analysis
A Student'southward t-test or a Wilcoxon's test were used to assess differences in the pre-operative and follow-upwardly clinical scores (AOFAS score and VAS for pain), later a normality examination (i.eastward. Kolmogorov-Smirnoff Z exam). The statistical significance level was set at p < 0.05. Analyses were performed using SPSS 20.0 for Windows (SPSS Inc., Chicago, Illinois).
Results
Thirty consecutive patients underwent full ankle replacement with a Zimmer TM TAR surgery between July 2013 to January 2016. At alphabetize procedure, 11 (37%) of cases included at least 1 concurrent procedure, and nineteen cases did not include any concurrent procedures (63%) (Table 1).
The mean preoperative FFI-hurting (FFI-P) value was 53.67, the FFI-inability (FFI-D) was 64.19. At the last follow-upwards visit, the FFI-P and FFI-D was sixteen.95 and xx.76 respectively (p<0.01 for the both scales). Preoperatively, the mean VAS for pain and AOFAS score was 7.81 and 40.95 respectively, and at the concluding follow-up two.29 and 86.38 p<0.01 for the both scales). The average postoperative tibiotalar ROM was eighteen.5 degrees in plantarflexion and 8 degrees in dorsiflexion.
The mean angle calculated using Forest and Deakin's method were "α" 89.02°, "β" 85.11 and "γ" 27.54 mail service-operatively. At the last follow-up the same values were respectively 89.43, 85.18 and 29.94 (p> 0.05 for the angles). At the last follow-upwardly, the mean offset ratio was 0.06 (range 0.003/-0.17). 10 percent was institute to be slightly anterior to the tibial axis and 3.three % (1 patient) posterior in the examined radiographs.
When assessing radiographs for subsidence/loosening, most implants prosthesis showed no radiographic evidence of cyst and/or lucency on either AP and/or lateral views except for iii patients with radiolucent lines in the inductive and posterior part of the tibia-prosthesis interface, one patient with radiolucent lines in the anterior office of the tibia-prosthesis interface and i patient with a medial malleolar cyst (Fig. 2).
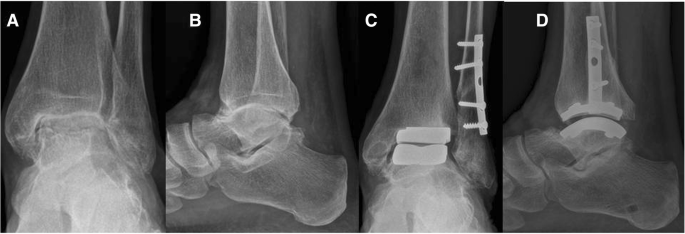
Pre-operative (a, b) and two-year follow-up weight bearing radiograph after Zimmer TM TAR showing a medial malleolar cyst (c, d)
Near patients (91%) were satisfied or very satisfied afterwards surgery and would take repeat the surgery if under the same conditions. The rate of major complications requiring surgery was 23.3 % (vii patients).
1 patient had a perioperative dislocation of the ankle (Fig. 3). Dislocation occurred the day subsequently implantation, during plaster cast positioning. At the mail service-operative radiography after cast positioning, the ankle was confused. Treatment consisted in open up reduction, syndemosis fixation and temporary fixation of the reduction with extrarticular kirschner wires. After reduction of the dislocation, we decided not to set up the medial malleolar since the construct was quite stable intra-operatively and considering a non-weightbearing cast was applied for six weeks. The reason for dislocation was missed diagnosis of the medial malleolar fracture during definitive components positioning: nosotros did not recognize the malleolar fracture at the final intra-operative radiographic control. Eighteen months later on surgery the patient underwent removal of the fibular plate and screws for skin irritation. Two months later hardware removal the patient complained mild hurting during walking and was satisfied with the outcome of the procedure.

Dislocation of the Zimmer TM TAR (a, b) with a undiagnosed intra-operative medial malleolar fracture, reduction and temporal fixation (c, d), half-dozen months follow-upwardly (e, f), one twelvemonth follow-up (g, h)
Vi patients underwent revision surgery. One patient adult a nonunion of the fibula that was therefore treated with autologous bone graft, plate fixation and medializing calcaneal osteotomy for residual hindfoot valgus. The patient did not present any factors for nonunion. A diagnosis of nonunion was made seven months after surgery based on clinical and radiological features. Wedlock was reached at iii months after surgery. The 2nd and third patient was yet reporting pain on the lateral side of the ankle joint i year after TAR with a residual varus deformity of the hindfoot. Nosotros performed a calcaneal Z osteotomy with Malerba'due south technique in the second patient and a Malerba's osteotomy associated with a dorsiflexory wedge osteotomy at the base of the first metatarsal in the 3rd patient. After iii months the patients had a significant clinical improvement and were very satisfied with the surgery. The fourth and fifth patient underwent hardware removal (fibular plate) 12 and 14 months respectively, subsequently the index surgery for pare irritation. The terminal patient underwent a medializing calcaneal osteotomy for symptomatic residual hindfoot valgus xiii months after TAR. The most common cause of hindfoot deformity correction after TAR was the pre-operative and intra-operative misjudgment of hindfoot alignment.
One patient adult an asymptomatic non-union, which did not require whatever farther treatment merely clinical and radiological follow-upwards.
1 patient that had rest hurting later on surgery is currently significant and therefore, nosotros are waiting, with her consent, earlier making farther radiographical analysis and revisional surgery. She has no functional deficit and the clinic is non susceptible of failure of the implant, loosening or infection and therefore the look and run across strategy seems, in our opinion, reasonable.
Discussion
Full ankle replacement is a common procedure with predictable results and is becoming increasingly more frequent for the treatment of talocrural joint osteoarthritis. Registry data from different countries take shown an increment in the apply of TAR for ankle osteoarthritis following traumatic upshot, rheumatoid arthritis and other atmospheric condition that cause a progressive loss of integrity of the tibio-tarsal joint [9].
In 2012 the Nutrient and Drug Administration approved a new type of prothesis: the Zimmer Trabecular Metal Total Ankle (Zimmer Inc.,Warsaw, IN). This implant was designed to allow the implant trough lateral approach. The main objective was to introduce a prosthesis that could decrease surgical complexity linked to delayed wound healing and to aid the surgeon who was more familiar with the lateral arroyo used for talocrural joint arthrodesis [ten]. Furthermore, this model is equipped with trabecular metal material, which was adult to simulate the normal architecture of the cancellous bone. Bobyn et al. have shown that the porous construction of this material permits os ingrowth in almost of the available surface, thus increasing the stability [xi]. Even though the prosthesis in the U.Due south. is implanted with cement fixation, it is ordinarily used off-label without cement and fixation relies on bony ingrowth at the bone-implant interface.
The hazard of wound healing issues is present in two-forty% of cases of TAR performed throw anterior arroyo [12, 13]. Early on TAR procedures had problems with wound healing but improvements in techniques, materials and postoperative intendance have reduced the incidence of infections. The percentage of incidence throw lateral approach should be theoretically lower due to the incision lying betwixt two angiosomes and therefore causing a small-scale vascular impairment of the skin.
The other main reward of a lateral approach is the possibility to have a direct visualization of the rotational center of the joint, and therefore allowing a more than accurate bone resection and reconstruction of the ankle joint anatomy and angles.
Some authors report the possibility of a major stability of the components due to the bone perpendicular orientation of the tibial and talar trabeculae that may improve the force transfer from implant and decrease the shear forces at the bone-implant interface [3]. Those data notwithstanding, don't take a statistical proof at the moment.
The complications of a lateral approach are associated to the fibular osteotomy with subsequent risk of delayed union, nonunion, change in fibular length, vascular and neural damage and painful hardware. Tennant et al reported the risk of lesion to the perforator peroneal artery during this approach in a cadaveric report [14]. Thus, the risk of blood vessels injury should be taking into business relationship.
In case of a revision a new osteotomy might exist necessary if the entire prosthesis must exist substituted, with an increased take chances of complications. If the damage is isolated to the polyethylene it might exist possible to do the exchange through anteromedial arthrotomy or lateral approach.
A report past Usuelli et al reported the possibility of a lower infection charge per unit in total ankle replacement trough lateral arroyo rather than anterior approach. The incidence was reported to be of 4.9% vs ii.9% for superficial infection and 3.7% vs one.iv% for deep infections, for the anterior and lateral approach respectively. Those differences were not found to be statistically significant [xv].
The survival charge per unit of the Zimmer TM TAR has been reported past few studies with insufficient follow-upward to be representative of the effectiveness of this prosthesis.
Barg et al. reported a 93% survival at 36 months with a decrease in VAS pain score from 7.9 ± 1.iii to 0.eight ± one.two after surgery [xvi]. Maccario et al. reported a 100% survival rate at 24 month and a decrease in VAS from 7.42 to i.42 [17]. Tan reported 20 cases of TAR through lateral arroyo with no failures during the first 12 months, proficient intra-operative alignment including viii patients (42.1%) with a hateful varus of 10.v± 4.2° and 4 (21.i%) with a mean valgus of 15.five± 8.half dozen° preoperatively. In both groups, the angles decreased to approximately two° postoperatively [xviii]. In a contempo newspaper, Usuelli et al. reported a 98.9 % survival charge per unit at 24 months with a rate of major complications requiring surgery of eleven.2 %. We plant in our patients a survival charge per unit of 100% with a decrease in VAS from 7.81 pre-operatively to 2.29 post-operatively and major complications charge per unit of 23.3 % [19].
In this report, four patients were younger than 40 years old. Younger patients testify higher activity level which tin theoretical influence polyethylene wearable. Therefore, an important business organisation in these patients is an expected college revision rate. In literature, at that place are no studies reporting high long-term survival (> 20 years) of TARs, and we therefore consider younger age a contraindication for TAR not through an accented age limit, but past taking into consideration the need of higher survivorship expectancy of the implants. When considering a younger patient for TAR, the possibility of future revisions through a revisional arthroplasty or salvage fusion, should be discussed.
A major concern with the lateral approach TAR is associated with fibular osteotomy and ligament sectioning [20]. DeVries et al. reported in a previous study of 16 patients with Zimmer TM TAR, good overall alignment even with valgus or varus hindfoot deformity [10]. However, 4 patients (25%) experienced complications related to the fibular osteotomy (non-union, delayed union, infection). In this study, fibular nonunion was nowadays in two patients and revisional surgery was necessary in one. We described also, the first post-operative case of ankle dislocation subsequently TAR. Despite the challenging handling, which included reduction and temporary fixation, good mid-term outcome was achieved at the last follow-upward. Considering these results, the lateral approach provides a good visualization of the joint but the hazard of fibular nonunion and instability should be kept in listen when considering this approach.
The major complication charge per unit in this written report (23.3%) was like to previous studies with different TAR systems. Hofmann et al. reported a major complication rate of 21% with the most common cause for reoperation of gutter impingement [21]. Nunley et. al reported 17% of patients requiring additional procedures later STAR system [22]. In a previous newspaper well-nigh Intramedullary-Fixation Total Ankle Arthroplasty (INBONE I/II), the reoperation rate due to postoperative complications in the short-term follow-upwardly was 24% [23].
Radiolucent lines are a cause for business afterward TAR. Barg et al. reported a loftier rate of radiolucent lines in the tibial and talar-implant interface of 34.five% and 12.7% respectively [24]. Interestingly, we observed radiolucent lines in 10% of the patients. Longer follow-upwards studies are warranted to understand the real nature of this radiological signs.
The radiographic angles used to assess component's migration were stable at the final follow-up and comparable to the results found by Haytmanek et al [25]. The authors reported a mean value of 87.5 for the α angle, 88.1 for the β angle and 17.four for γ angle.
The clinical results of this group of patients are like to the results for pain outcomes reported in the meta-assay past Zaidi et al., in which the mean pooled summary VAS scores decreased from seven.iv preoperatively to 1.six postoperatively [26]. In a previous paper by Usuelli et al. the AOFAS hindfoot score of 67 patients increased from 32.eight to 85.0 [27].
In a previous study, Hsu assessed the clinical outcomes with use of AOFAS ankle-hindfoot score after both INBONE I and II total ankle arthroplasties [23]. The mean overall improvements in the AOFAS score was 43.two points with nearly of the patients very satisfied with the concluding issue. Nunley reported a hateful alter in the AOFAS summary score of 52 points, afterwards the STAR arthroplasty [22]. We report similar results with an increase from 40.95 to 86.38 with a hateful increase of 45.22 (range from 26 to 57).
We admit the limitations of this written report due to the low number of patients, its retrospective nature and express follow-up time.
Conclusion
In this study, patients reported high levels of satisfaction with a low incidence of complications related to the lateral approach. Most of the patients reported an increase in the AOFAS score and a subtract in FFI-P, FFI-D and VAS for hurting score.
Abbreviations
- AOFAS:
-
American Orthopedic Human foot and Ankle Society
- ATFL:
-
Anterior talofibular ligament
- FFI-D:
-
Foot Office Index- Inability
- FFI-P:
-
Foot Part Index- Pain
- GCT-TS:
-
Behemothic cell tumor of the tendon sheath
- ROM:
-
Range of movement
- TAR:
-
Total ankle replacement
- VAS:
-
Visual Analouge scale
- Zimmer TM TAR:
-
Zimmer Trabecular Metal Total Talocrural joint Replacement
References
-
Daniels TR, Younger AS, Penner G, et al. Intermediate-Term Results of Total Ankle Replacement and Talocrural joint Arthrodesis. J Bone Jt Surgery-American Vol. 2014;96(2):135–42.
-
Raikin SM, Rasouli MR, Espandar R, Maltenfort MG.Trends in treatment of advanced ankle arthropathy by full ankle replacement or anklefusion. Foot Ankle Int. 2014;35(3):216–24.
-
Tan EW, Maccario C, Talusan PG, Schon LC. Early Complications and Secondary Procedures in Transfibular Total Ankle Replacement. Foot ankle Int. 2016;37(8):835–41.
-
Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders G. Clinical Rating Systems for the Ankle-Hindfoot, Midfoot, Hallux, and Bottom Toes. Foot Ankle Int. 1994;15(7):349–53.
-
Martinelli Due north, Scotto GM, Sartorelli E, Bonifacini C, Bianchi A, Malerba F. Reliability, validity and responsiveness of the Italian version of the Foot Office Index in patients with pes and talocrural joint diseases. Qual Life Res. 2014;23(one):277–84.
-
Wood PLR, Prem H, Sutton C. Total talocrural joint replacement: Medium-term results in 200 scandinavian total ankle replacements. J Bone Jt Surg - Br Vol. 2008;90-B(5):605–9.
-
Wood PLR, Deakin S. Total ankle replacement. The results in 200 ankles. J Os Joint Surg Br. 2003;85(three):334–41.
-
Barg A, Elsner A, Chuckpaiwong B, Hintermann B. Insert Position in 3-Component Total Ankle Replacement. Pes Ankle Int. 2010;31(nine):754–nine.
-
Roukis TS, Prissel MA. Registry data trends of total ankle replacement use. J Foot Ankle Surg. 52(6):728–35.
-
DeVries JG, Derksen TA, Scharer BM, Limoni R. Perioperative Complications and Initial Alignment of Lateral Arroyo Total Ankle Arthroplasty. J Foot Talocrural joint Surg. 2017;56(5):996–one thousand.
-
Bobyn JD, Stackpool GJ, Hacking SA, Tanzer K, Krygier JJ. Characteristics of bone ingrowth and interface mechanics of a new porous tantalum biomaterial. J Bone Articulation Surg Br. 1999;81(5):907–14.
-
Mroczek K, Mroczek K. Perioperative Complications of Total Ankle Arthroplasty. Myerson MS, ed. Foot Ankle Int. 2003;24(1):17–21.
-
Pyevich MT, Saltzman CL, Callaghan JJ, Alvine FG. Total Ankle Arthroplasty: a Unique Design. Two to Twelve-yr Follow-up*. J Os Joint Surg Am. 1998;eighty(ten):1410–20.
-
Tennant JN, Rungprai C, Pizzimenti MA, et al. Risks to the claret supply of the talus with four methods of total talocrural joint arthroplasty: a cadaveric injection written report. J Bone Articulation Surg Am. 2014;96(five):395–402.
-
Usuelli FG, Indino C, Manzi L, Maccario C, Vulcano Eastward. Superficial and Deep Infections Charge per unit in Primary Total Ankle Replacement through Anterior Approach versus Lateral Transfibular Approach. Foot Ankle Orthop. 2017;2(3):2473011417S0003.
-
Barg A, Saltzman C. Early Clinical and Radiographic Outcomes of Trabecular Metallic Total Ankle Using Transfibular Approach. Foot Ankle Orthop. 2017;ii(3):2473011417S0001.
-
Maccario C, Indino C, Manzi L, Usuelli FG, Di Silvestri C. Transfibular Full Talocrural joint Replacement Consequence at 2 Years Follow Up. Foot Talocrural joint Orthop. 2017;2(3):2473011417S0002.
-
Tan EW, Maccario C, Talusan PG, Schon LC. Early Complications and Secondary Procedures in Transfibular Full Ankle Replacement. Foot Talocrural joint Int. 2016;37(8):835–41.
-
Usuelli FG, Maccario C, Granata F, Indino C, Vakhshori V, Tan EW. Clinical and Radiological Outcomes of Transfibular Total Talocrural joint Arthroplasty. Foot Talocrural joint Int. 2018;eleven:1071100718798851.
-
Martinelli N, Bianchi A, Romeo G, Malerba F. Alphabetic character Regarding: Early Complications and Secondary Procedures in Transfibular Total Ankle Replacement. Pes Ankle Int. 2016;37(10):1149.
-
Hofmann KJ, Shabin ZM, Ferkel E, Jockel J, Slovenkai MP. Salto Talaris Total Talocrural joint Arthroplasty: Clinical Results at a Mean of 5.2 Years in 78 Patients Treated by a Unmarried Surgeon. J Bone Joint Surg Am. 2016;98(24):2036–46.
-
Nunley JA, Caputo AM, Easley ME, Cook C. Intermediate to long-term outcomes of the STAR Total Talocrural joint Replacement: the patient perspective. J Bone Joint Surg Am. 2012;94(1):43–8.
-
Hsu AR, Haddad SL. Early clinical and radiographic outcomes of intramedullary-fixation full ankle arthroplasty. J Bone Joint Surg Am. 2015;97(iii):194–200.
-
Barg A, Bettin CC, Burstein AH, Saltzman CL, Gililland J. Early Clinical and Radiographic Outcomes of Trabecular Metal Total Talocrural joint Replacement Using a Transfibular Arroyo. J Bone Joint Surg Am. 2018;100(half-dozen):505–15.
-
Haytmanek CT Jr, Gross C, Easley ME, Nunley JA. Radiographic Outcomes of a Mobile-Bearing Total Ankle Replacement. Pes Ankle Int. 2015;36(ix):1038–44.
-
Zaidi R, Cro S, Gurusamy M, Siva North, Macgregor A, Henricson A, Goldberg A. The outcome of total ankle replacement: a systematic review and meta-analysis. Os Joint J. 2013;95-B(11):1500–7.
-
Usuelli FG, Indino C, Maccario C, Manzi Fifty, Salini V. Total ankle replacement through a lateral approach: surgical tips. Sicot-J. 2016;2:38.
Acknowledgements
Not applicable.
Funding
Expenses related to the publication fees of the nowadays article were supported by the Italian Ministry building of Wellness. No funding were used in the design of the study and collection, analysis, and estimation of data and in writing the manuscript.
Availability of data and materials
All information are bachelor without restriction contacting the respective authors (NM). Data are available from the internal registry of IRCCS Istituto Ortopedico Galeazzi, Milano, Italy, upon Ethics Commission approving for researchers who meet the criteria for access to confidential data.
Writer data
Affiliations
Contributions
Each author has participated sufficiently in the work: JF, CM and NM, reviewed the radiographic examinations, performed the statistical assay and wrote the newspaper; NM and AB performed the surgical interventions and the clinical evaluations; NM, FM and MH, participated in the design of the study and supervised the draft of the paper; FG assisted in writing, provided study materials and approved the final version of the article. All the authors read and canonical the manuscript.
Corresponding writer
Ideals declarations
Ideals approving and consent to participate
This retrospective report was approved by our ethical committee (San Raffaele Hospital,76/int/2017) and a written informed consent was obtained from all patients.
Consent for publication
All individuals involved in this study provided written consent to use their clinical and imaging data for enquiry purposes.
Competing interests
Dr. Nicolò Martinelli works as an Associate editor for BMC Musculoskeletal Disorders.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Admission This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in whatsoever medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Eatables license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zip/ane.0/) applies to the data made available in this commodity, unless otherwise stated.
Reprints and Permissions
About this article
Cite this article
Bianchi, A., Martinelli, North., Hosseinzadeh, M. et al. Early on clinical and radiological evaluation in patients with total ankle replacement performed by lateral approach and peroneal osteotomy. BMC Musculoskelet Disord 20, 132 (2019). https://doi.org/x.1186/s12891-019-2503-half-dozen
-
Received:
-
Accepted:
-
Published:
-
DOI : https://doi.org/10.1186/s12891-019-2503-half dozen
Keywords
- Ankle arthroplasty
- Ankle osteoarthritis
- Pain
- Total ankle replacement
Source: https://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/s12891-019-2503-6
0 Response to "Zimmer Total Ankle Replacement Reviews Vs Hintermann Series H2ã‚â® Total Ankle Replacement System"
Post a Comment